As of late, I’ve posted a fair amount about the local politics involved with the various tax-funded emergency services districts in my part of Texas basically ending volunteer participation. Truth be told, I definitely think there’s some shenanigans from paid staff and their union locals. But folks, if we’re going to talk about the end of volunteer participation, we need to take a long hard look at the volunteer culture.
As I often teach through sarcasm, I present the following recommendations for ways to ensure that your volunteer department becomes a combination department and eventually a completely paid department.
- Run the department as your own private social club. By gosh, this is a place for the connected locals to hang out, use as a private lounge, and maybe go travel on someone else’s dime.
- Training? Why do it? And if you do feel you have to do it, focus on cool, fun stuff instead of the basics of being able to operate at a fire, rescue, or medical call.
- Membership? Who needs that? If people want to join us, they’ll find us. And if they do figure out how to join the department, ensure that the process is all about who you know rather than what you’ll bring to the department. And if you do a membership drive, make it a joke. Either try to recruit “heroes” (as opposed to members who want to help others) or do the same tired routine that you do every so often and then claim “nothing’s working.”
- Speaking of what you bring to the department, always make sure to turn down free help. If the person can’t make the arbitrary number of meetings or responses, or lives “too far,” don’t show any flexibility. If you’re a combination fire and EMS organization, be sure to turn down someone only interested in one discipline. It’s not like having an extra medic frees up a firefighter or vice versa.
- Accountability and transparency is for the birds. You’re heroes! There’s no need to justify your budget or be accountable to those politicians at the county or the city who “don’t understand what we do.”
- Speaking of budgets, let’s be sure to spend like drunken sailors on shore leave. Buy those big-ticket, rarely used capital expenditures regularly, then run around scavenging for IV needles and working radios.
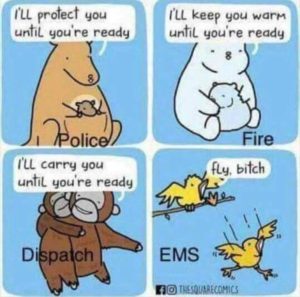
- Responses? We’re volunteers. We don’t have to go to a call if we don’t want to. And we sure don’t go to “old so-and-so’s” house or the local nursing home. It’s not like they really need help. And especially if you have paid staff working with the volunteers, there’s no need to go to all calls, only the fun ones. And if you show up on the fun calls and don’t get to do “fun” stuff, by all means, complain loudly.
- Uniforms? They need to fall into one of two extremes. Either no uniforms and look like “People of Wal-Mart” or uniforms that make you look like an Italian Field Marshal. No need for things like photo ID cards, t-shirts, polo shirts, and jackets. It’s either the Redneck Yacht Club or the full parade dress.
- Be sure to remind new members that they don’t know how “we do things around here.” Be especially unwelcoming to experienced people who have significant prior experience. It’s not like they bring anything to the table.
- Don’t create strong relationships with the other members of the public safety team. No need to play well with the surrounding fire or EMS agencies, much less law enforcement. It’s not like you’ll ever need any of these guys again.
- And if you have a state organization for volunteer fire and EMS, don’t join it. And if you do end up joining said organization, ensure that your organization is quiet at the state capitol. We don’t want to antagonize the paid guys or advocate for volunteers.
So, if you follow my program, what will you get? Simple. Eventually, the taxing entity and taxpayers will tire of your antics. They will point to your lack of training, transparency, fiscal responsibility, and shrinking membership roster. First, they’ll bring on a small duty crew during the day to “supplement” the volunteer staffing. Eventually, that supplement supplants the volunteers. And somewhere during this process, your department becomes absorbed by the taxing entity. Congratulations! Your non-profit volunteer group has now become a fully paid local government department. But of course, the fun only begins. All of the time and effort that you could’ve spent on having a functional volunteer or combination department can now be spent on lengthy political and legal battles over who gets the property from your department.
This story repeats itself over and over again, yet we don’t seem to learn. The average volunteer emergency services provider is often their own worst enemy and the biggest reason why departments go “professional.”
And so it goes.